a) How to order for blood transfusion:
The following steps should be followed
- Assess patient's clinical need for blood
- Inform patient's relatives about the proposed transfusion and record it.
- Record the indications for transfusion.
- Select the blood product and quantity required.
- Complete the blood request form accurately and legibly.
- Obtain and correctly label a blood sample for compatibility testing.
- Send the blood request form and blood sample to the blood bank.
- Laboratory performs pre-transfusion antibody screening and compatibility tests and
selects compatible units.
- Delivery of blood products by blood bank or collection by clinical staff.
b) What to do with received blood units:
It is essential to store blood products in correct storage conditions if not immediately
required for transfusion.
During transfusion check the identity on: Patient, Blood product, Patient's documentation
During administration of the blood product, it is essential to record in the patient's
notes.
- Type and volume of each product transfused
- Unique donation number of each unit transfused
- Blood group of each unit transfused
- Time at which the transfusion of each unit commenced
- Signature of the person administering the blood.
Monitor the patient before, during and on completion of the transfusion. Record
the completion of the transfusion. Identify and respond immediately to any adverse
effect. Record any transfusion reactions in the patient's notes.
c) How to administer blood and blood components:
Whole Blood and Red Cells
Should be stored in the ward or operating theater refrigerator at 2°C to 6°C until
required for transfusion ( 6°C = minimize the growth of any bacteria , 2°C = prevent
haemolysis, which can cause fatal bleeding problems or renal failure).
Whole blood and red cells should be infused within 30 minutes of removal from refrigeration.
Platelet Concentrates
Are stored at room temperature of 20-240C (Platelet concentrates that are held at
lower temperatures lose their blood clotting capabipty hence they should never be
placed in a refrigerator)
They should be transfused as soon as possible after issue.
Fresh Frozen Plasma and Cryoprecipitate
Fresh frozen plasma should be thawed in the blood bank in accordance with approved
procedures and it should be infused within 30 minutes of thawing.
If not required for immediate use, it should be stored in a refrigerator at a temperature
of 2°C to 6°C and transfused within 24 hours (As with whole blood or red cells,
bacteria can propferate in plasma held at room temperature)
Check the compatibility label
The following things should be checked:- Blood pack no, Patient's name, Patient's
hospital reference number or date of birth, Patient's ward, Patient's ABO and RhD
group, Expiry date, Date of compatibility test, Blood group of blood pack.
During administration of the blood products
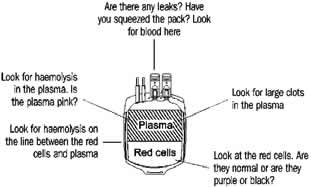
1. Check the blood pack for signs of deterioration specially when
- On arrival in the ward or operating room.
- Before transfusion, if it is not used immediately.
2. Check for
- Discoloration or signs of any leakage
- Any sign of haemolysis in the plasma
- Any sign of haemolysis on the line between the red cells and plasma.
- Any sign of contamination - change of colour in the red cells. (darker or purple/black
)
- Any clots (blood was not mixed properly with anticoagulant / bacterial contamination
due to the utilization of citrate by proliferating bacteria )
- Any signs that there is a leak in the pack or that it has already been opened.
Do not administer the transfusion if the blood pack appears abnormal, damaged or
has been (or may have been) out of the refrigerator for longer than 30 minutes.
Inform the blood bank immediately.
The Final Patient Identity Check
- Final identity check should be undertaken at the patient's bedside immediately before
commencing the administration of the blood product.
- It should be undertaken by two people, at least one of whom should be a registered
nurse or doctor.
- Ask the patient to identify himself/herself by family name, given name, date of
birth and any other appropriate information If the patient is unconscious, ask a
relative or a second member of staff to state the patient's identity.
- Check the patient's identity and gender and Check the details on the compatibility
label.
- There should be no discrepancies between the ABO and RhD group on blood pack and
compatibility label.
- Check that there are no discrepancies between the unique donation number on blood
pack and compatibility label.
- Check that the expiry date on the blood pack has not been passed.
The final check at the patient's bedside is the last opportunity to detect an identification
error and prevent a potentially incompatible transfusion, which may be fatal.
Time Limits for infusion:
|
Component
|
Start infusion
|
Complete infusion
|
|
Whole blood / red cells
|
Within 30 mins of
removing pack
from refrigerators
|
Within 4 hrs
|
|
Platelet concentrates
|
immediately
|
Within 20 mins
|
|
FFP & CP
|
As soon as possible
|
Within 20 mins
|
Disposable equipment for blood administration
For infusion of whole blood, red cells, plasma, platelets and cryoprecipitate
- Use a new, sterile blood administration set
- Change the set at least 12-hourly during blood component infusion
- In a very warm climate, change the set more frequently and usually after every four
units of blood, if given within a 12-hour Period.
In Pediatrics patients
- Use a special pediatric set for pediatrics patients, if possible. These allow the
blood or other infusion fluid to flow into a graduated container built into the
infusion set. This permits the volume given, and the rate of infusion, to be controlled
simply and accurately.
Warming of blood
There is no evidence that warming blood is beneficial to the patient when infusion
is slow.
- At infusion rates greater than 100 ml/minute, cold blood may be a contributing factor
in cardiac arrest. However, keeping the patient warm is probably more important
than warming the infused blood.
- Warmed blood is most commonly required in large volume rapid transfusions ( In adults:
infusion greater than 50 ml/kg/hour, In children: infusion greater than 15 ml/kg/hour)
- Exchange transfusion in infants
- Patients with clinically significant cold agglutinins.
It is important to note that
- Blood should only be warmed in a blood warmer.
- Blood should never be warmed in a bowl of hot water as this could lead to haemolysis
of the red cells which could be life-threatening.
Pharmaceuticals and blood products
- Do not add any medicines or any infusion solutions other than normal saline (sodium
chloride 0.9%) to any blood component.
- Use a separate IV line if an intravenous fluid has to be given at the same time
as blood components.
Recording
- Before administering blood products, it is important to write the reason for transfusion
in the patient's case-notes.
- If the patient later has a problem that could be related to the transfusion, the
records should show who ordered the products and why. This information is also useful
for conducting an audit of transfusion practice.
- The record you make in the patient's case-notes is your best protection if there
is any medico-legal challenge later on.
Monitoring of patient
- Before commencing the transfusion, it is essential to encourage the patient to notify
a nurse or doctor immediately if he or she becomes aware of any reactions such as
shivering, flushing, pain or shortness of breath or begins to feel anxious. Ensure
that the patient is in a setting where he or she can be directly observed.
Monitoring the transfused patient
For each unit of blood transfused, monitor the patient:
Before starting the transfusion, as soon as the transfusion is started, 15 minutes
after
starting the transfusion, at least every hour during transfusion, On completion
of the
transfusion and 4 hours after completing the transfusion.
At each of these stages, record the following information on the patient's chart:
Patient's general appearance, Temperature, Pulse, Blood pressure, Respiratory rate,
Fluid balance, Oral and IV fluid intake and Urinary output.
Record:
- Time the transfusion is started
- Time the transfusion is completed
- Volume and type of all products transfused
- Unique donation numbers of all products transfused
- Severe reactions are most commonly present during the first 15 minutes of a transfusion.
All patients and, in particular, unconscious patients should be monitored during
this period and for the first 15 minutes of each subsequent unit.
Acute transfusion reactions
- If the patient appears to be experiencing an adverse reaction, stop the transfusion
and seek urgent medical assistance. Record vital signs regularly until the medical
officer has assessed the patient.
- In the case of a suspected transfusion reaction, do not discard the blood pack and
infusion set, but return them to the blood bank for investigation.
- Record the clinical details and actions taken in the patient's case-notes.